Paralysis ticks are a silent but deadly killer, and unfortunately, Australia’s climate is the perfect breeding ground for them.
Animal Emergency Service (AES) is one of Queensland’s leading hospitals when it comes to treating tick paralysis. Dr Rob Webster, a registered specialist in Emergency Medicine and Critical Care, is not only one of the founders of AES, but also a member of the Australian Paralysis Tick Advisory Panel. Dr Rob and the AES team have treated tens of thousands of patients suffering from tick paralysis over the last two decades.
This guide on tick paralysis provides information on the dangers of ticks, how to know if your pet has been affected and practical tips on keeping your pet safe during tick season.
What you’ll learn
- What are paralysis ticks?
- Where can paralysis ticks be found?
- What do paralysis ticks look like?
- What are the symptoms of tick paralysis?
- What should you do if your pet shows these symptoms?
- Are there any other ticks my pet can get?
- Prevention
- Treatment
- Patient stories
What are paralysis ticks?
The paralysis tick (ixodes holocyclus) is a small eight-legged, egg-shaped arachnid, approximately 3-5mm in length. Their appearance does vary depending on their life-stage.

While only small they are a dangerous parasite that injects a potentially fatal toxin (holocyclotoxin) into the bloodstream while feeding on mammals, both native and domestic animals. This toxin can lead to a number of symptoms, causing severe illness and can potentially result in death. It is important to note both dogs and cats can be affected, however native animals are not.
Where can paralysis ticks be found?
Paralysis ticks are found along coastal parts of central and southern Queensland as well as coastal New South Wales. Towards the north, paralysis ticks can be found all year-round, while further south tick season generally begins in winter (August) and finishes in late spring (November). However, this is not a set period. For example, tick season may start earlier if the winter is milder than usual.
Australia is the most diverse country in the world for ticks, with over 70 species, several of which look like the paralysis tick but are actually harmless. It is recommended that if a tick is found on your pet, you should quickly visit your vet to identify the species.
The paralysis tick is common in woodlands and grasslands. Cats and dogs will be exposed to ticks if they go anywhere which is frequented by wild animals, including bandicoots and possums. While they don’t fly or jump, they will climb or drop onto a pet’s coat when they brush past where the tick is sitting.
What do paralysis ticks look like?
The paralysis tick can look different depending on whether it has fed or not. As the paralysis tick feeds, they become engorged with blood changing colour from white-ish to blue-ish/light grey colour.

Once a tick attaches to an animal, it deeply and firmly embeds itself into the skin. The area where the tick has attached itself will become red with a raised thickening, which is also referred to as a crater.

What are the symptoms of tick paralysis?
While Australian wildlife have some immunity to the tick toxin, cats and dogs are very susceptible and will develop paralysis, breathing difficulty, which, in severe cases, can lead to death if they are exposed to a tick.
There are a number of symptoms to look out for. The early stages of a paralysis tick bite can be hard to determine as they are typically vague. As symptoms quickly progress from the initial bite, they become more severe.
Dr Brooke Schampers explains what tick paralysis is, and the signs and symptoms to be aware of
Early vague stages of tick paralysis can include the following symptoms:
- Lethargy
- Reduced appetite
- Occasional vomiting
If you see any of these symptoms, search your pets for ticks immediately and contact your vet, as from these initial symptoms their condition can rapidly deteriorate.
Other symptoms of tick paralysis include:
- A change in the sound of the bark or meow. For example, becoming softer or changes in pitch.
- Cannot blink. If ticks become attached near the eyes the eyelids can become paralysed which means they are unable to blink. This can then lead to the eyes drying out and becoming damaged.
- Difficulty breathing or rapid breathing. As the paralysis advances the muscles used in breathing become weak. Heavy breathing can occur, this can involve panting, noisy breathing and at times grunting and coughing.
- Change in heart rhythm or rate.
- Excessive drooling. Paralysis can lead to difficulty swallowing which lead to a build-up of fluid in the mouth and throat.
- Wobbly gait, which often starts off from the back legs.
- Reluctant to move, stand or jump.
- Completely paralysed.
Paralysis ticks can cause wobbly gait, which usually starts with the back legs being effected
What should you do if your pet shows these symptoms?
If you believe your pet is experiencing any of these symptoms take your pet to your vet or nearest emergency centre immediately. Early treatment is thought to be a key element of successful recovery from tick paralysis and deterioration can occur in a short space of time, often within hours. Animals exhibiting any of the symptoms of a tick bite, such as paralysis and breathing difficulty require immediate treatment. However, the early signs are often subtle and may occur singly, such as vomiting and reduced appetite, and therefore easily to go unnoticed without a professional assessment.
By taking your pet to the vet immediately after showing symptoms of a tick bite, the veterinarian will be able to complete a focused examination which will include a search for additional ticks. It has been found that 10% of patients will have more than one tick. Tick preventatives can also be administered.
If you do find a tick, keep your pet quiet and calm, and at a comfortable temperature. Search for any ticks and remove them if able. If a tick is removed prior to visiting a vet, it is important to bring the tick along with you so the species can be identified. It is important not to provide food or water as if your pet has been affected by a paralysis tick, they will be unable to protect their airway when they swallow. This may lead to food or water being breathed into their airways which can cause aspiration pneumonia and serious breathing difficulties. Do not use chemicals to remove ticks or try burning the tick off.
Even if a tick is removed it is still important that you take your pet to a vet. Pets can continue to worsen up to three days after a tick has been removed. The poison ticks inject remains active in the pet’s system for 1-2 weeks after it has been removed.
Find out more about the paralysis tick, symptoms and what happens to paralysis tick patients in the hospital.p
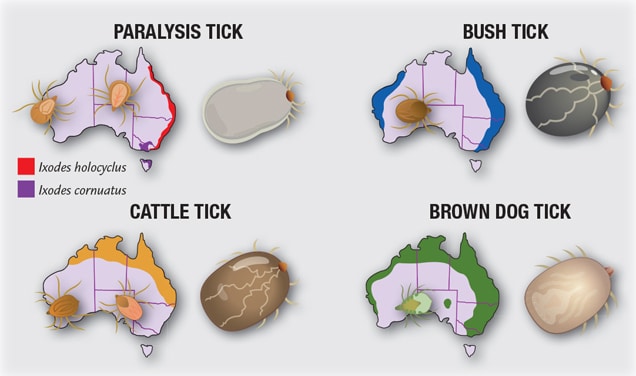
Are there any other ticks my pet can get?
There are other ticks to be on the look out for. Two species of ticks in particular can also be a cause for concern.

They are commonly found in the environment of the animal they attach themselves to. For example, the kennel in the backyard or inside the home.

They can be found in rural or semi-rural areas with a hot or humid climate.
If you are not sure about ticks in your area, contact your vet.
Prevention
Prevetnion is always better than a cure.
As the leading specialist in tick prevention and treatment, Animal Emergency Service sees over 3,500 tick cases each year, most of which can be prevented.
Animal Emergency Service’s Dr Rob believes it is entirely possible to eradicate the number of tick cases, through preventative measures and staying vigilant.
“I’m on a mission to eliminate tick paralysis.” – Dr Rob Webster

The elimination of tick paralysis is possible through preventative methods and daily searches of your pet. There are several methods to help prevent your pet from contracting a paralysis tick, which can be administered all year-round.
Tick preventatives
- Routinely administer tick preventatives to your cats and dogs as they may be susceptible to tick paralysis, even if they have suffered from it before
- Seek veterinary advice on which tick preventative is most appropriate for your pet
- Use the most effective product for your pet’s lifestyle, for example, if your pet is regularly bathed or goes swimming, avoid using a product that needs to be spread on the coat
- Ensure the preventative medication you are using offers protection against paralysis ticks
- Read the label instructions and administer accordingly i.e. the correct dose for your pet‘s weight at the appropriate dosing interval (e.g. monthly)
- If you are travelling to a known tick area, seek veterinary advice regarding when you need to administer the tick preventative prior to departure, and after your return
- Have your pet’s coat clipped short to make locating ticks easier
- Avoid taking your pet walking in areas with lots of wildlife

Daily searches of your pets for ticks
- If you live in, or you and your pet are visiting a known tick area, it is recommended to search your pets daily for ticks and tick craters
-
If you or your pet have recently travelled to a known tick area, continue these daily searches for at least one week after your return
-
When administering a search for ticks it is best to start at the front end of your pet. A review of over 2,000 cases found 90% of tick paralysis were found forward from the shoulders
-
Technique:
-
Start searching for ticks at the front end of your pet and move towards the back of the body. For example, start at the nose, moving to the mouth, eyes, ears (including inside the ears), neck, chest, front legs (extending down to the paws and between and underneath their toes), back, body and belly, hind legs, prepuce/vulval areas and the full length of the tail
-
Remove your pet’s collar to search for ticks that may be under the collar
-
Using your fingertips, gently move them or ‘fingerwalk’ between the fur at the level of the skin, over every aspect of your pet
-
If you find a tick or tick crater, continue searching the entire body of your pet in case more tick(s) are attached
-
If your pet has a long coat, consider clipping your pet (including head and tail) during periods of high tick risk to make searching and detection of ticks easier
-
Animal Emergency Service’s Dr Brooke Schampers, along with her fur baby Polo, show us how to conduct a tick search
Reduce the tick population at home
- Minimise or restrict your pet’s access to bushy environments
- Discourage wildlife from entering your property by installing fences
- Clean up leaf litter
- Clear tall grass and brush around the house and at lawn edges
- Keep grass mowed where possible and mow frequently
- If you store wood outside, stack neatly in a dry area
- Keep play equipment, decks and patios away from yard edges and trees
- Remove old furniture or rubbish from the yard as this reduces available hiding places
- If you live adjacent to wooded or bushy areas create a protective barrier of mulch around the perimeter of your property. This creates a physical barrier that is dry and sometimes hot, which ticks cannot tolerate.
- Vacuuming regularly will help remove ticks hiding in carpet that have been dragged in from the outdoors.
Cat specific prevention
It is a myth that cats don’t get ticks. Cats are less likely to get ticks than dogs, but it can still happen. There are a multitude of products available for dogs for tick prevention from collars, spot-ons, tablets, and rinses. Cats, however, are not afforded the same luxury of choice. Due to a peculiarity in the liver metabolism of cats, they are very sensitive to one of the insecticides that are present in most of the tick products currently available. This chemical is permethrin which is highly toxic to cats.
Learn more about the precautions needed when preventing tick paralysis in cats.

Please ensure to consult with your regular vet about what tick prevention products and methods they recommend.
Tick paralysis treatment
The good news is that tick paralysis can be treated and most (but sadly not all) animals will recover. If your pet has been exposed to a paralysis tick, please note that the symptoms (worsening paralysis, regurgitating or vomiting, change in voice and breathing difficulties) can occur or worsen for up to three days after the tick is removed.
Virtually all animals that show symptoms will need treatment. The first step is to call your vet immediately after identifying potential symptoms.
Secondly, remove the tick from your pet’s skin at home. Leaving the head in is not a disaster – it does not continue to pump poison and will eventually fall out (leaving a crater) after just a few days.
The third step is to get them to your closest emergency vet. See where all Animal Emergency Service locations are located.
Once your pet has been admitted to the hospital, they will undergo diagnostics, treatment and then constant monitoring by our vets and nurses. The treatment process for tick paralysis can vary drastically from patient to patient. Initial treatment varies depending on whether the assessment determines the patient to be stable or unstable.
Dr Brooke Schampers takes you into our hospital and explains how we treat tick paralysis, and the preventative measures you can take
What to expect from the vet
- Sedation to help calm your pet. Pets get very distressed when they cannot move or have trouble breathing. Sedation will help in removing any anxiety
- Oxygen therapy if having difficulty breathing
- Emergency intubation and manual ventilation
- If your pet is having a lot of trouble breathing, either from severe paralysis or there is vomit inside the lungs (aspiration pneumonia)
- A tube is placed down your pet’s airways and a nurse will breathe for them
- Tick search and removal of any remaining ticks
- Medications
- Tick antiserum
- Antibiotics (if suspected lung infection from breathing in vomit)
- Blood tests
- Assess your pet’s ability to breath
- Monitor hydration status and electrolyte levels (commonly lost through vomiting)
- X-rays
- If your pet is having trouble breathing
- Intensive nursing care
- Your pet won’t be able to urinate as their bladder is paralysed; a nurse will need to help empty their bladder regularly
- To help change your pet’s position to prevent pressure sores since they cannot move
- Medications for your pet’s eyes when they cannot blink to prevent development of eye ulcers
- Multiple tick searches throughout hospital stay
- Full-body tick clip – this helps in finding further ticks
- Anti-parasitic shampoos to eliminate any remaining ticks, in case they are too small to be found by hand
- Mechanical ventilation
- For pets too paralysed to breathe
- For pets with such severe lung disease they cannot breathe (from breathing vomit into their lungs)
Patient stories
While prevention methods outlined above are quite effective, sometimes the worst can happen, and a paralysis tick can result in a trip to the emergency vet.
Animal Emergency Service has had tens of thousands of tick paralysis cases over the years, ranging from short stays to life-threatening conditions. Find out more about how we treat tick paralysis cases.
Lucca’s story
In some severe cases patients require a mechanical ventilator to ensure oxygen continues to flow through the patient’s lungs while they are unable to do so themselves. One of the brave Animal Emergency Service patients, Lucca, went through this process.
One afternoon Lucca’s owners noticed that he had become wobbly on his back legs, Lucca’s quick-thinking owners checked him all over and found a paralysis tick on his leg. They removed the tick and jumped in the car straight away to seek veterinary help.

He was taken to his primary vet where he was admitted for treatment. Unfortunately, tick paralysis is an unpredictable condition and Lucca quickly deteriorated despite the initial treatment. Lucca was rushed to the Pet Intensive Care Unit (Pet ICU) at Underwood via animal ambulance. On arrival at Pet ICU, Lucca was placed on life support and remained in an induced coma for three days while the paralysis wore off and his lungs grew stronger. Read more about Lucca’s story.

Bella’s story
Another memorable case was when a cute little Maltese Terrier named Bella was admitted to us in a bad way. She was unable to stand up and had difficulty catching her breath. Bella’s owner had suspected a tick was causing the problem and knew what to look for but did not find the tick despite several searches. Ticks can be very difficult to find, even in dogs with short hair, let alone a Maltese Terrier with a beautiful coat.
Bella was admitted to hospital, and the AES team gave her the life-saving tick antiserum. This is essential even if the tick has been removed. Ticks can inject a lethal dose of toxin into a pet by the time the first signs of wobbliness begin in the legs. Without treatment, a pet can die despite removing the tick. Read more about Bella’s story.

If your pet has a tick or you suspect they do, contact your closest Animal Emergency Service hospital or your local vet immediately.
For more information about what is toxic to pets, visit our Pets and Poisons Guide.
